USC Stem Cell
News
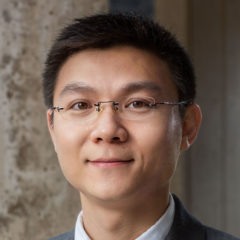
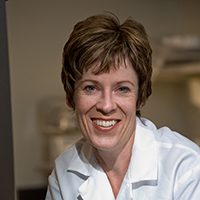
view all newsMeet Our Researchers
Find Education and Training Opportunities
Explore Research Facilities
Learn About Our Research
Videos
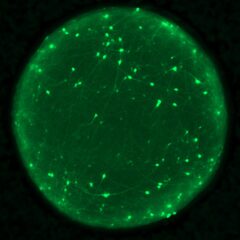
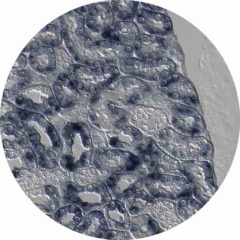
The Lindström lab is hiring: Dr. Nils Lindstrom's lab studies the molecular mechanisms that control how progenitors that exist during development differentiate into the broad range of cell types that underpin adult kidney function.
view all videos